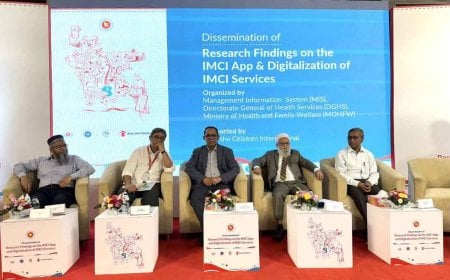
Integrated Intervention Improves Nutrition Among Urban Poor, Study Finds

Around 80 percent of pregnant women and 58 percent of those living in Dhaka’s urban slums suffer from calcium and iron deficiencies, respectively, according to a new study by the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b). The findings suggest that integrated services can significantly improve nutritional outcomes for marginalized urban populations.
The results were presented on Monday, July 7, at the Sasakawa Auditorium of icddr,b, based on research conducted in the Bauniabadh slum of Mirpur under the Nutri-Cap program. Researchers observed that children in these slums are generally underweight and stunted. “There is vast inequality among urban populations, with nearly half of the slum dwellers living in food insecurity, and about 50 percent of the children being stunted,” the researchers noted.
Conducted under the Advancing Sexual and Reproductive Health and Rights (ADSARCH) initiative, the study focused on the nutrition and hygiene status of low-income pregnant women, adolescent girls, and children under two years of age living in urban slums.
The icddr,b researchers highlighted that while Bangladesh has made remarkable progress in healthcare over the last two decades, rapid urbanization has created new challenges. The urban population has surged from 8 percent in 1973 to 40 percent in 2022, now totaling 62 million people. This number may double by 2035. Although urban areas generally perform better in health indicators compared to rural ones, the stark income disparity has resulted in deep inequality. For instance, while 53 percent of urban women receive at least four antenatal care visits from trained providers, the figure drops to 40 percent among slum residents. Moreover, nearly one-third of the slum population is under 15 years of age, indicating the urgent need for targeted nutritional interventions.
The Nutri-Cap initiative identified 721 pregnant women among 15,000 married women in Bauniabadh during the study period. It also included 4,200 adolescent girls and around 2,500 children under two. In-depth analysis was conducted from November 2021 to February 2022 on 2,826 households out of 16,532 surveyed. Despite some stability, poverty and hardship remained acute. The average monthly income was BDT 21,000, yet one in every four families experienced food insecurity, and 91 percent of these were indebted. In 39 percent of the households, more than three people shared one sleeping space. Women contributed to the household income in 42 percent of families, and just over one-third had completed primary education.
The Nutri-Cap model delivered a package of services to three vulnerable groups: pregnant women, adolescent girls, and young children. Pregnant women received monthly home visits that included nutrition counseling, supplements such as iron, folic acid, calcium, and vitamin D, as well as monitoring of weight, blood pressure, hemoglobin, and blood sugar. They were encouraged to attend regular antenatal checkups and take adequate rest.
The outcomes were promising. Average weight gain among pregnant women in the program was 8.9 kg, compared to 7.5 kg in the comparison group. Rates of safe delivery and hospital births increased, while incidences of miscarriage, stillbirths, and neonatal deaths declined. The risk of delivering underweight babies dropped by 16 percent.
Among adolescents, average hemoglobin levels rose from 12 to 12.8 g/dL. Although there was no significant change in food diversity, awareness of nutrition and health improved. Of the adolescent girls, 14.9 percent were undernourished and 12.6 percent overweight—figures in line with national urban averages.
Children in the program also showed substantial improvements in growth, with reduced rates of stunting and underweight. Biological tests showed that inflammation in the gut among adolescent girls had decreased, while immunity had improved.
The study also demonstrated economic efficiency. While the program required more time investment, overall healthcare costs fell, particularly for medications and diagnostics for pregnant women and children. Human resource costs were the highest, but researchers noted that if the model is institutionalized, it could be cost-effective in the long run.
Lead researcher Dr. Mostafa Mahfuz emphasized that community involvement was key to the program’s success. “The model worked because it listened to the community, trained local women, and tackled multiple challenges simultaneously. The combination of compassion and evidence-based programming creates limitless possibilities,” he stated.
icddr,b Executive Director Dr. Tahmeed Ahmed added, “Slum dwellers have long been neglected in basic healthcare services. Adapted models like Nutri-Cap are not only effective but scalable across other urban slums and even in international contexts.”
The seminar opened with remarks by Dr. Thaddeus David May, Senior Director of the Nutrition Research Division at icddr,b, and concluded with Dr. Shams El Arifeen, Project Director of ADSARCH by icddr,b and Professor Emeritus at icddr,b, who emphasized the need for broader expansion and partnership of the model.
Government officials, development partners, NGO representatives, and researchers from various sectors participated in the seminar.